Many our clients are using Telehealth during this Coronavirus pandemic.Whether you are new to telemedicine or you have been using it for years, we thought you might be interested in some of the “rules” that apply, including HIPAA compliance.
HIPAA rules have been relaxed during the COVID-19 Emergency
Medicare Guidelines
- As of March 17, 2020, the restrictions have been lifted to perform Telemedicine services. These can be either simple audio or they can include video.
- Qualifications and Patient Consent. The person providing Telehealth services must be an MD, NP or PA.
The practitioner (MD, PA, NP) shall provide the member (patient) with the basic information about the services that he/she will be receiving via telehealth, and the patient must provide his/her consent to participate in the telehealth services. The consent must be documented.
Telehealth services/sessions shall not be recorded without the patient consent. - Video. If the Telehealth session is video, they are Synchronous Telehealth Services, defined as “live video-conferencing,” which is a “two-way audiovisual link between a patient and a care provider.”
- Equipment. For Synchronous Telehealth services: The provider (MD, PA, NP) must document what equipment they are using and that they made the patient aware of the method. Telehealth services can be allowed or utilized with certain smart phones. If the patient and the MD have a smart phone, they can utilize them if the phones have video and audio capabilities enabling real two-way encounter.
- Scope of Practice & Carrier Requirements. Providers must be acting within their scope of practice and some carriers require the patients to sign up for Telemedicine services. Please check with your carriers or call Jennifer Church at 631-203-1370 at Fellow Health Partners for help in determining which ones patients to sign up.
- Whether the patient is receiving ongoing treatment via telehealth or is a new patient, the member (patient) must be informed of the following patient rights and policies.
- Established Patients Only. HHS will not conduct audits checking the patient’s status as the waiver only allows for established patient
Telemedicine: Update from Fellow Health Partners (cont’d)
- Although many telephone services are exempt from copays, it’s not so clear with telehealth services. Some carriers will apply a co pay but most won’t. The provider may reduce or waive the patient co pays without having a financial hardship agreement.
- Documentation and Coding: The Provider must document the equipment used for the call, where the patient is located and where the provider is located. They must document the time as the codes are time related.
- The Provider must have appropriate S.O.A.P. notes (Subjective, Objective, Assessment, and Plan.)
- There are Telephone E&M codes that can be used.
- The following codes apply.
- 99441: Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5 – 10 minutes of medical discussion
- 99442: Telephone evaluation and management; 11-20 minutes of medical discussion
- 99443: Telephone evaluation and management; 21-30 minutes of medical discussion
- These E&M codes are billable for telehealth services with these modifiers.
- 99202-99205 New Patient
- 99212-99215 Established patient
- Modifiers:
- 95 Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System.
- GT: Via interactive audio and video telecommunication systems (for Commercial Medicare carriers and Medicare)
- GQ: Via asynchronous telecommunications system (not happening at the same time, transmission of patient health care data, recorded video, it is to provider to provider. (we would have no need for this.) This is in the event a provider sends consulting information to another provider.
The POS code that we bill with is 02.
- Reminder: These are all time related codes and the time must be documented in the patient note, along with the assessment of the patient, the diagnosis.
Telemedicine: Update from Fellow Health Partners (cont’d)
- If there is a failure of transmission the providers must have a written policy detailing a contingency plan in the case of a failure of transmission or other technical difficulty that renders the service undeliverable.
- If the service is undeliverable because of transmission failure you cannot submit any claims to Medicare/Medicaid and or other carriers.
From the CMS fact sheet:
EXPANSION OF TELEHEALTH WITH 1135 WAIVER: Under this new waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence starting March 6, 2020. A range of providers, such as doctors, nurse practitioners, clinical psychologists, and licensed clinical social workers, will be able to offer telehealth to their patients. Additionally, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs
Medicare beneficiaries will be able to receive a specific set of services through telehealth including evaluation and management visits (common office visits), mental health counseling and preventive health screenings. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, are able to visit with their doctor from their home, without having to go to a doctor’s office or hospital which puts themselves and others at risk.
You can go to this website for additional information on the telehealth services for CMS:
https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-providerfact-sheet
More details on equipment and other legal issues can be found here:
https://www.healthlawattorneyblog.com/telehealth-remote-communications-during-covid-19/
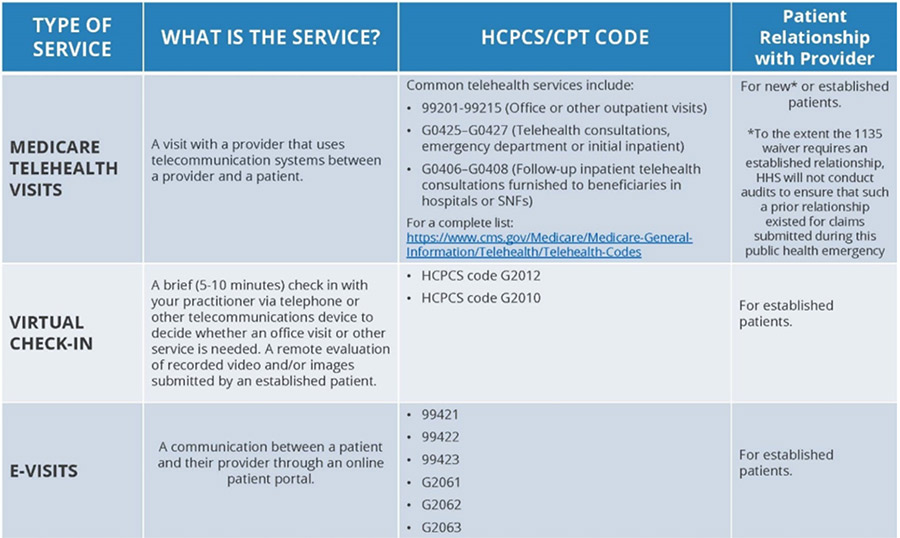
See chart on the next page for the Types of Service covered.